In New Zealand, around 1 in 8 Kiwi adults and 1 in 7 Kiwi children suffer with a respiratory disease. For children, asthma is one of the most common causes of hospital admissions. On Average, 77 Kiwis die from asthma each year.
Currently there is no cure for asthma, however there are lots of things you can do to manage it better so that it doesn't impact on your life too much. The first step is to learn as much as you can about the condition and the steps you can put in place to control it.
What is asthma?
Symptoms of asthma
- Chest tightness
- Wheeze
- Cough
- Shortness of breath
What is a trigger?



- Animals (cats, horses)
- Dust mites
- Moulds
- Pollens
- Foods
- Cold/flu
- Exercise
- Cigarette smoke
- Temperature changes
- Medications
- Dust
- Perfumes
- Chemicals
- Food additives
- Laughing/crying
- Emotional stress
- Occupational
- Air pollution/smog/fumes
- Strong smells
- Pre-menstrual hormone changes
Is your asthma well controlled?
- Do you experience shortness of breath, cough or wheeze with exercise?
- Are you needing to use your reliever more than two times a week on a regular basis?
Take our quiz to find out if your child's asthma is well controlled.
- There are no or minimal asthma symptoms
- You know which asthma triggers to avoid
- The reliever medication is used less than 2 times a week
- You do not regularly wake in the night with a cough/wheeze
- You do not miss days off school or work because of asthma
- You are reviewed by your GP every 6 months
What is a reliever and what is a preventer?

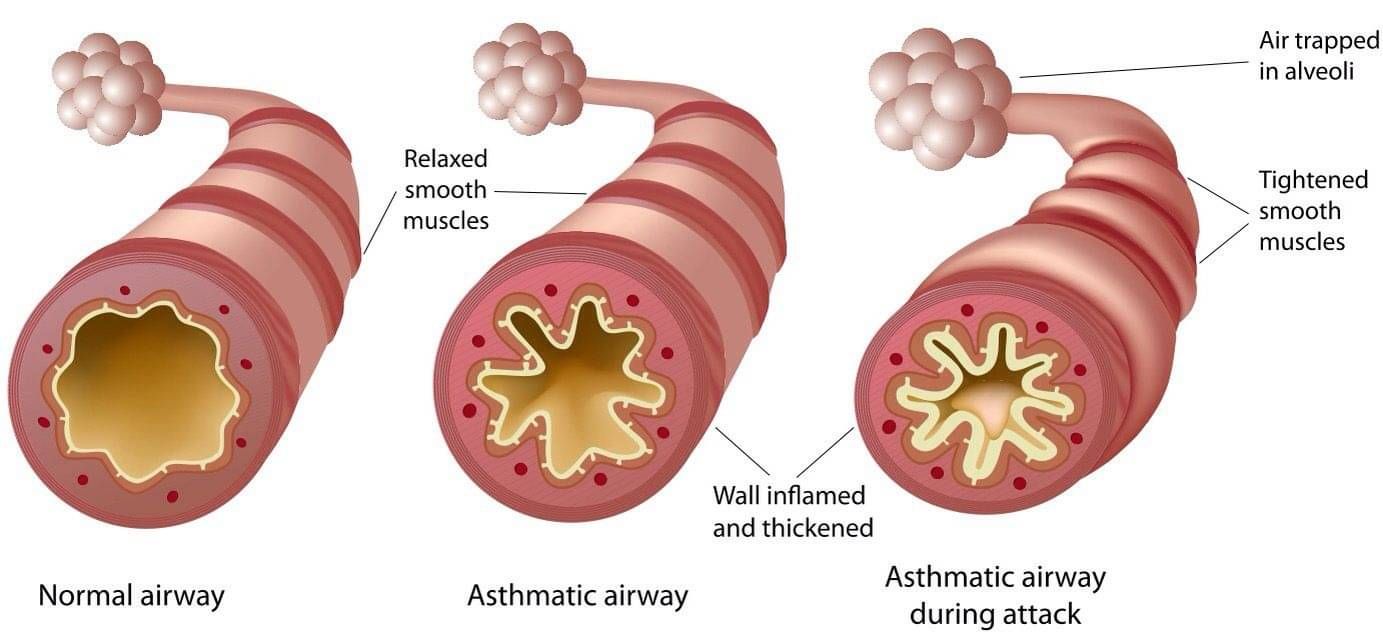
Reliever medication works quickly, enabling you to continue your daily routine. However, the reliever does not prevent the lining on the inside from becoming swollen causing risk of blockage and limitation of airflow.
Preventer medication works very slowly, over a period of days to months to reduce the inflammation and sensitivity. Preventers need to be taken every morning and night, every day, even when well to be effective. Preventers are a long term medication that should not be stopped but may be gradually reduced under your doctor's supervision.
Why too much reliever isn't a good thing.
Many people are overly reliant on their reliever (usually blue or grey) inhaler. But most do not realise that overusing this medication can actually cause more harm than good. It is a brilliant first aid medicine but doesn’t actually treat the underlying problem. And if you need to use it more than twice a week then this indicates your asthma isprobably uncontrolled. Have a watch of this video to learn more about this.
What is a spacer?
Spacers are clear plastic tubes with a mask or mouthpiece on one end and an opening to insert the inhaler into at the other end.
Spacers are not just for kids! Using an MDI (puffer) with a spacer delivers up to 50% more medicine to your lungs than using a puffer alone. Why? Because spacers slow down the speed of the medicine coming out of the inhaler, suspending it briefly in the chamber, making it easier to breathe in. Using a puffer without a spacer means the majority of the medicine ends up hitting the back of the throat, resulting in an increased risk of thrush and other oral problems. It also means a reduced amount of medicine is getting to the lungs where it is needed.

'With a Spacer' and 'Without a Spacer'.
Cleaning your spacer
They should be washed weekly and left to drip dry. This is important to reduce medicine build up on the inside of the chamber which hinders effectiveness. If spacers are left to retain condensation, mould or mildew can grow creating a very unhealthy device to breathe through. If debri is inside the mouth piece and cannot be removed during washing discard the spacer and replace with a new one. You can request a replacement from your medical centre which you are enrolled in or purchase one at a pharmacy.
How to wash your spacer
- Remove base only from the spacer
- Wash them in warm soapy water (nothing scratchy)
- DO NOT rinse the bubbles out, DO NOT towel dry
- Leave on the bench to AIR DRY
- Replace base once dry
- Spacer is now ready to use
NOTE
- Spacers should be changed every 6 – 12 months. Tiny scratches and abrasions on the inside of the spacer can reduce the effectiveness of the medicine delivery
- One puff in the chamber at a time, to 6 breaths. Numerous puffs in the chamber at once will cause the particles to clump together and become harder to breath in hence resulting in ineffectiveness.
Administration techniques
An MDI (Puffer Inhaler)
How to Use - Correct Technique:
- Shake medication
- Insert into base end of spacer
- Place lips around mouth piece to create a seal
- Press MDI once
- Breathe in and out normally through the mouth 6 times
- For further doses, repeat steps 1-5
- Listen for the "butterfly" valve clicking when you breathe in and out (with the e-chamber model)
- Replace after 12 months of use
When to wean off the mask and why
Children aged 1-4 generally use a mask with the spacer. During the ages of 2-4 transition to using the spacer mouthpiece directly in the mouth without the mask can begin. A good seal around the mouthpiece with the lips is essential. This transition is important as up to a third of the medicine can be lost on the face when using a mask, meaning less medicine reaching the lungs where it is needed. However, during this time of transition the mask may still be needed in times of acute flare-ups as a good seal around the mouthpiece may not be possible.
A Turbuhaler
How to Use - Correct Technique:
- Twist – unscrew and remove the cover.
- Hold the turbuhaler upright and twist the grip as far as it will go in both directions until you hear a click. The turbuhaler is now loaded with one dose of medicine
- Breathe out away from the turbuhaler – do not blow directly into your turbuhaler
- Place the mouth piece in your mouth and form a good seal with your lips and breathe in deeply.
- When finished place the cover back on the inhaler and twist shut.
Remember - load like a rocket and inhale like a plane
The most common mistakes with the turbuhaler
- Not holding the turbuhaler upright when priming
- Covering the air inlets with lips
- Breathing in through the nose instead of mouth
- Shaking the turbuhaler to see how much is left
- Storing the inhaler in a damp environment with the cap off.

Spacers are free at Asthma Waikato or your GP surgery (Pharmacies may charge).
Do you need to know more about Asthma? Need to see a Educator?
Are you struggling with your asthma? Alternatively, you have ideas of how we might be able to help you help us continue working with people and families in the Waikato with asthma or COPD? Whatever it is, please don't hesitate to get in touch.







